In the ever-evolving landscape of cancer treatment, one of the most groundbreaking developments has been the emergence of immune checkpoint inhibitors. These drugs have revolutionized the way we approach cancer care, offering new hope to patients with previously untreatable conditions. As part of the broader field of immunotherapy, checkpoint inhibitors harness the body’s own immune system to target and destroy cancer cells. This article explores what these drugs are, how they work, and their impact on modern medicine.
Understanding Immune Checkpoint Inhibitors
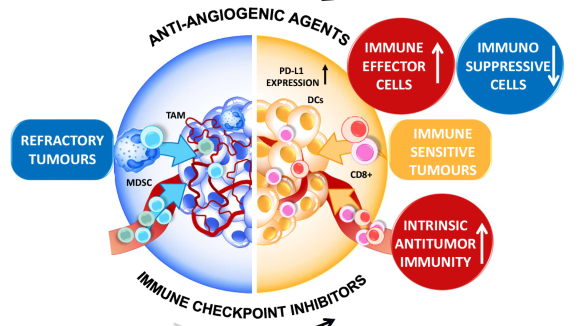
Immune checkpoint inhibitors are a type of immunotherapy designed to enhance the immune system’s ability to fight cancer. The term “checkpoint” refers to the natural mechanisms that regulate the immune system to prevent it from attacking healthy cells. However, cancer cells can exploit these checkpoints to evade immune detection and continue growing unchecked.
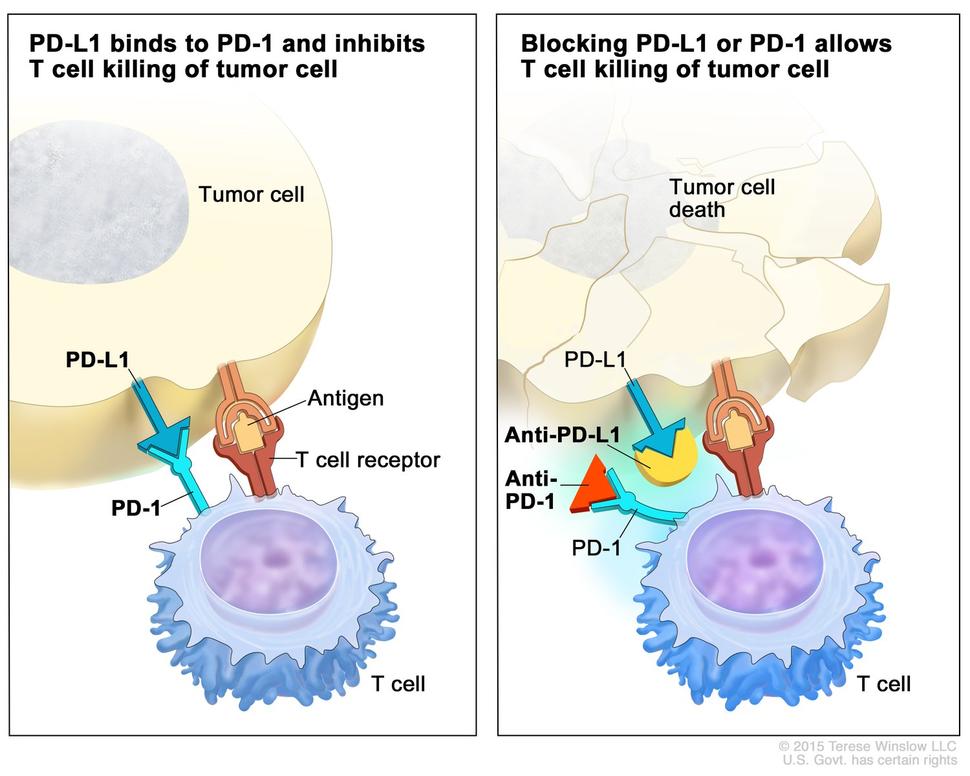
By blocking specific proteins—known as checkpoints—on immune cells or cancer cells, these inhibitors effectively “take off the brakes” and allow the immune system to recognize and attack cancer more effectively.
These drugs are named after the specific checkpoint proteins they target. Common examples include:
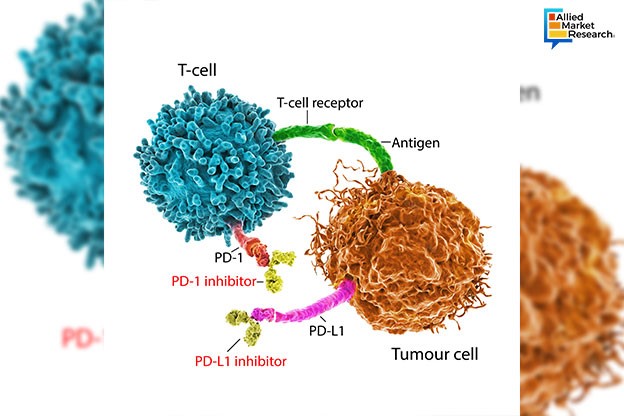
- PD-1 inhibitors (e.g., nivolumab, pembrolizumab)
- PD-L1 inhibitors (e.g., atezolizumab, durvalumab)
- CTLA-4 inhibitors (e.g., ipilimumab)
Each of these drugs works slightly differently, but all aim to restore the immune system’s ability to detect and eliminate cancer cells.
How Do Checkpoint Inhibitors Work?
To understand how checkpoint inhibitors function, it’s important to first grasp the role of T cells in the immune system. T cells are a type of white blood cell that plays a critical role in identifying and destroying infected or abnormal cells, including cancer cells.
However, T cells have checkpoints—proteins that act like switches to turn the immune response on or off. For example:
- PD-1 is a protein found on the surface of T cells. When it binds to PD-L1 (a protein often found on cancer cells), it signals the T cell to stop attacking.
- CTLA-4 is another checkpoint protein that prevents T cells from becoming overactive.
Cancer cells can take advantage of these checkpoints by expressing high levels of PD-L1 or other checkpoint proteins, essentially hiding from the immune system. This is where checkpoint inhibitors come into play. By blocking these proteins, the drugs remove the “brakes” on the immune system, allowing T cells to recognize and attack cancer cells more effectively.
This process is not without risks, however. Because checkpoint inhibitors boost the entire immune system, they can sometimes cause autoimmune reactions, where the immune system attacks healthy tissues. Managing these side effects is a key focus of ongoing research.
Types of Cancers Treated with Checkpoint Inhibitors
Checkpoint inhibitors have shown remarkable success in treating several types of cancer, particularly those that were once considered difficult to manage. Some of the most common cancers treated with these drugs include:
- Melanoma (skin cancer)
- Non-small cell lung cancer (NSCLC)
- Hodgkin lymphoma
- Kidney cancer
- Bladder cancer
- Head and neck cancers
- Bile duct cancer
- Breast cancer
- Stomach cancer
For example, nivolumab and pembrolizumab have been approved for use in melanoma, lung cancer, and Hodgkin lymphoma, while ipilimumab has been effective in treating advanced melanoma. Atezolizumab and durvalumab are used in lung and bladder cancers, respectively.
The effectiveness of these drugs varies depending on the type and stage of cancer, as well as the individual patient’s condition. Researchers are continuously exploring ways to expand the use of checkpoint inhibitors to treat more cancer types.
The Future of Checkpoint Inhibitors
While checkpoint inhibitors have already made a significant impact, there is still much to learn about their long-term effects and optimal use. One of the biggest challenges is determining which patients will benefit most from these treatments. Currently, only about 20 to 25% of patients respond positively to checkpoint inhibitors, highlighting the need for better predictive tools.
Researchers are also investigating combination therapies, where checkpoint inhibitors are used alongside other treatments such as chemotherapy, radiation, or vaccines. These combinations may help improve outcomes and reduce resistance.
Another area of interest is the development of personalized immunotherapy, where treatments are tailored to the unique genetic makeup of each patient’s tumor. This approach could lead to more effective and targeted therapies with fewer side effects.
Experts like Dr. Gordon Freeman, a pioneer in this field, believe that within the next decade, 60% of cancer patients could benefit from immunotherapy. With continued research and innovation, the future of cancer treatment looks increasingly promising.
Conclusion
Immune checkpoint inhibitors represent a major breakthrough in the fight against cancer. By leveraging the power of the immune system, these drugs offer new hope for patients who previously had few options. While challenges remain, the progress made so far has already transformed the lives of many individuals, including those like Jay Schwab, who benefited from these life-saving treatments.
As research continues, the potential for even greater advancements in this field is immense. Whether through improved drug formulations, combination therapies, or personalized approaches, the future of cancer care is bright—and it starts with the immune system.
Author: Sarah Thompson
Title/Role: Health and Science Journalist
Credentials: With over a decade of experience covering medical advancements, Sarah has reported on breakthroughs in oncology, immunology, and public health. She holds a Master’s degree in Journalism from Columbia University and has contributed to leading health publications.
Profile Link: https://www.sarathompsonhealth.com
Sources:
– Dana-Farber Cancer Institute
– National Institutes of Health (NIH)
– American Cancer Society
Internal Links:
– Understanding Immunotherapy
– Latest Cancer Treatments
– How Vaccines Work
Call to Action:
Stay updated with the latest news on cancer research and treatment advancements. Explore today’s headlines and discover how science is changing lives.
URL Slug: us-trending-news-immune-checkpoint-inhibitors
Image Optimization:
–
– 
– 
– 
– 
Schema Markup:
{
"@context": "https://schema.org",
"@type": "Article",
"headline": "US Trending News: What Are Immune Checkpoint Inhibitors and How Do They Work in Cancer Treatment?",
"datePublished": "2025-04-05",
"dateModified": "2025-04-05",
"author": {
"@type": "Person",
"name": "Sarah Thompson"
},
"publisher": {
"@type": "Organization",
"name": "Health Insights Today",
"logo": {
"@type": "ImageObject",
"url": "https://www.sarathompsonhealth.com/logo.png"
}
},
"description": "Learn how immune checkpoint inhibitors are transforming cancer treatment and improving patient outcomes."
}
Featured Snippet Optimization:
Immune checkpoint inhibitors are a type of immunotherapy that helps the immune system fight cancer by blocking proteins that prevent T cells from attacking cancer cells. These drugs are used to treat various cancers, including melanoma, lung cancer, and Hodgkin lymphoma.







More Stories
67 Emote Clash Royale Emote: Complete List and Guide
What Is the 504 Gateway Timeout Error and How to Fix It?
US Trending News: 67 Emote Clash Royale QR Code: How to Use and Where to Find It